
Understanding Chronic Myeloid Leukemia
What is Chronic Myeloid Leukemia?
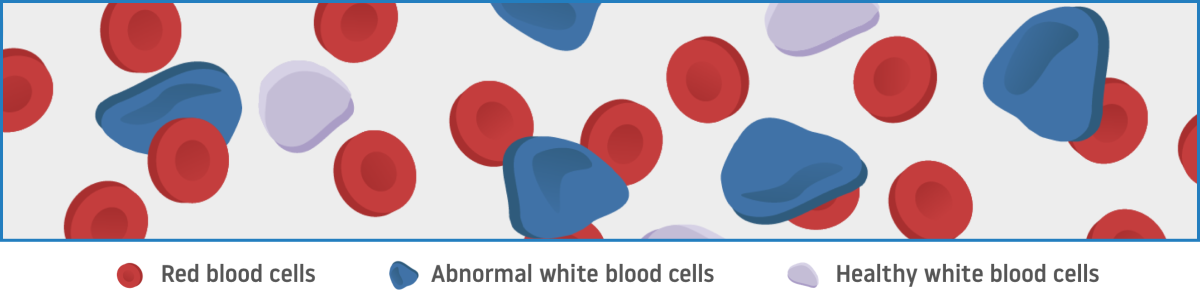
Chronic myeloid leukemia (CML) is a type of blood cancer in the bone marrow that causes too many white blood cells to form. It starts with an abnormal change, or mutation, in a cell’s DNA that creates a chromosome known as the Philadelphia (Ph) chromosome.
- When the Ph chromosome is present in cells, a protein known as BCR::ABL1 is produced
- The BCR::ABL1 protein causes the bone marrow to produce abnormal white blood cells
- These abnormal cells are CML cells. Over time, they overtake healthy white blood cells in the bone marrow to cause leukemia
In CML, abnormal cells crowd out healthy cells in the bone marrow
Phases of Chronic Myeloid Leukemia
There are 3 phases, or stages, of CML that represent different levels of progression: chronic phase, accelerated phase, and blast phase, which range from least to most severe:

Not actual patients
CML treatment may include chemotherapy and/or a type of targeted therapy called a tyrosine kinase inhibitor (TKI)
CML treatment with TKI therapy
Many people with CML are treated with a type of targeted therapy known as a tyrosine kinase inhibitor, or TKI. The protein that causes CML, BCR::ABL1, is a tyrosine kinase protein. The TKIs used to treat CML specifically inhibit BCR::ABL1. They help stop abnormal white blood cells, or CML cells, from forming in the body.
Monitoring your response to treatment
The goal of CML treatment is to keep your levels of BCR::ABL1 as low as possible. This can help reduce the number of CML cells in your body. Your doctor may do molecular or cytogenetic tests on cells from your bone marrow or blood to see how well a treatment is working.
One term your doctor may use to describe the results of these tests is log reduction. This is a measure of how much BCR::ABL1 levels have been lowered. Log reductions typically mean that a treatment is working well to control CML.
Mutations and treatment resistance
Understand the role mutations may play in treatment resistance.